Any pathologist who has diagnosed a breast cancer case knows all too well how arduous and inefficient mitotic counting can be, while at the same time how critical it is not only to diagnosis, but to deciding the treatment pathway that will follow. So, it is essential that pathologists get it right. Yet pathologists are only human, and humans can make mistakes – especially when trying to identify small cell structures under a microscope and manually quantify them. Magnify this with the time and resource pressures pathology labs are facing today, and the challenge only grows. This is where artificial intelligence (AI) can provide great value.
AI – in healthcare as in any other field – works best when used alongside the human’s existing skillset to accelerate painstaking tasks and enhance productivity. For this reason, AI represents the perfect solution for allowing pathologists to more efficiently identify and quantify mitoses, which would provide welcomed help to pathologists, oncologists, and patients alike. And, though adoption of digital pathology and AI is only beginning to really accelerate in labs around the world, this is not a far-away goal; This is the next era of breast cancer diagnosis, and it’s here today.
Why Has Mitotic Counting Remained a Challenge?
Historically, mitotic counting has been done by examining a glass slide under a microscope to try to find a ‘hotspot,’ or an area with the highest density of mitoses, and then counting each of these mitoses by hand. This leaves quite a bit of room for subjectivity, as finding the hotspot itself can be difficult and open to individual interpretation. There are also many structures that can resemble mitoses and differentiating them from true mitoses is challenging even for experienced pathologists. Once true mitoses are found, it is time-consuming and painstaking to count them and provide an accurate estimate of the mitotic density per square millimeter of cancerous tissue.
The driving force behind each of these challenges is not a lack of pathologist skill, but that it is being done on a microscope. Since different microscopes have different field areas, which leads to variability and lack of standardization, the microscope is not the optimal tool for mitotic counting. Digital pathology, on the other hand, facilitates this task by offering a wide, unobstructed viewing pane that enables the view of the entire slide. It also enables the use of digital tools like counters, area grids, and improved annotation tools, which further streamline this task. Importantly, digitization is also a prerequisite to AI, which can additionally help to dramatically enhance the efficiency and accuracy with which pathologists find hotspots and mitoses and potentially accelerate turnaround times, all of which help ensure patients are positioned to achieve the best possible treatment outcomes.
How Does Paige’s AI Help?
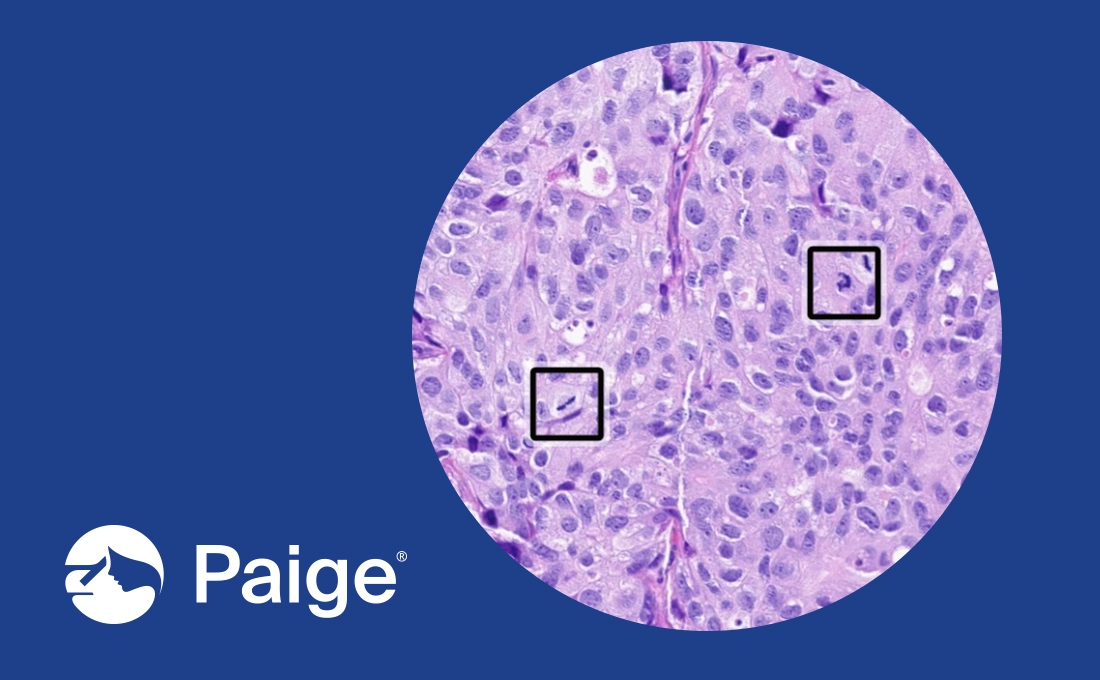
Paige Breast Mitosis was specifically designed to address the exact, longstanding challenges pathologists often face when finding and counting mitoses. First, it helps to intelligently identify a hotspot, which can drastically reduce the subjectivity that tends to arise at this step. It then allows pathologists to view the hotspot on a TissueMap, which highlights the hotspot without blurring out the surrounding tissue so they can easily assess it in context, adding a level of decision-making confidence. Within the hotspot, Paige Breast Mitosis will also draw a square around each individual mitosis it has detected, helping to draw pathologists attention to the right areas on the slide and make manual counting far more efficient and seamless. It even offers the ability to see the automatically calculated quantity of mitoses on the entirety of the slide as well as the quantity within the pre-identified hotspot (calculated per 2mm2) with a click, so pathologists can finalize their diagnosis with unparalleled efficiency and confidence.
Each of these features supports pathologists in streamlining the aspects of mitotic grading they find the most tedious or challenging, while giving them the space to spend their time and skill where it is most needed. When used in conjunction with pathologists’ skill, the application can help reduce diagnostic turnaround time and enhance overall grading precision, both of which would be valuable to ensuring patients get timely and effective care.
Importantly, Paige Breast Mitosis is uniquely able to help pathologists achieve these outcomes because it was built using 4 critical elements; robust training data, rigorous testing and internal validation, and pathologist-centric design. Paige leverages our exclusive access to a diverse dataset of over 5 million whole-slide images to build each of our applications. In the case of Paige Breast Mitosis, the application was trained on over 8,000 individual mitoses, pulled from slides representing patients and staining protocols from across the globe. This not only ensures that the application is able to deliver high performance in any lab setting, but that it is tuned to encompass the breadth of complexity and variability real patient cases will contain.
The application also underwent extensive testing by our internal team of experts along with practicing pathologists from a variety of practice types, and to date, we continue to work with these real-world pathologists to independently validate its performance regularly and thoroughly. We also designed the application’s features based on direct feedback from pathologists to ensure it fits the realities of clinical practice, can help resolve ongoing challenges, and seamlessly supports clinicians in delivering timely patient care with confidence.
Ultimately, however, for true transformation to occur in pathology, the creation of quality AI alone is not enough. Labs must begin to take steps to complete a digital transformation that will enable their use of these AI tools within day-to-day practice. This will not only ensure that their labs are equipped to keep pace with the changing landscape of cancer care that AI will usher in but will bring never-before-seen efficiencies and confidence to cancer diagnosis that will help all patients around the world get access to the highest quality care when they need it. With digital transformation, pathologists can put themselves at the forefront of the new era of cancer care, ensuring that the many benefits of AI are realized in real-world practice for the benefit of patients.
—
In the European Union & United Kingdom, Paige Breast Mitosis is CE-IVD & UKCA marked. In United States and where research use is permitted, Paige Breast Mitosis use is limited to Research Use Only and not for use in diagnostic procedures.